Key Takeaways
Clinical History
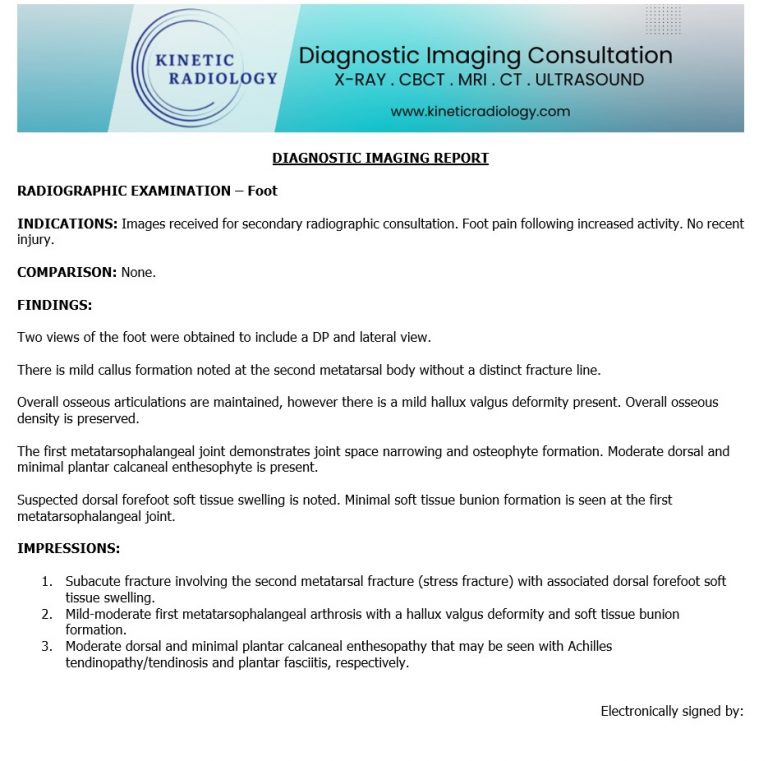
A 32-year-old male marathon trainee complains of insidious onset of forefoot pain, specifically over the mid-to-distal second digit. No acute trauma reported. The patient recently increased his weekly running volume from 20 miles to 45 miles over a three-week period. Pain is exacerbated by weight-bearing and relieved by rest.




Diagnosis: Subacute Second Metatarsal Stress Fracture (Diaphyseal)
A subacute diaphyseal stress fracture of the second metatarsal is a hairline break along the shaft of the bone caused by repetitive mechanical loading rather than a single traumatic event. It commonly occurs in athletes, military recruits, or individuals with sudden increases in activity. In the subacute stage, imaging may show cortical thickening, periosteal reaction, or a visible fracture line, reflecting ongoing bone remodeling. Patients typically present with localized dorsal foot pain that worsens with weight-bearing and improves with rest.
A metatarsal stress fracture is a fatigue fracture, occurring when “normal bone is subjected to abnormal, repetitive stress.” This differs from an insufficiency fracture, where “abnormal bone (e.g., osteoporosis) is subjected to normal stress.”
Biomechanical Failure
In distance runners, the bone undergoes a constant cycle of micro-damage and repair. According to Wolff’s Law, bone adapts to the loads placed upon it. However, if the rate of osteoclastic resorption (removing damaged bone) exceeds the rate of osteoblastic deposition (laying down new bone), the cortex weakens.
The second metatarsal is particularly vulnerable because it is the most rigid part of the forefoot. During the late stance phase of gait, the second metatarsal acts as a pivot. If the first ray (the big toe) is dysfunctional—as seen in our patient with 1st MTP arthritis—the normal “windlass mechanism” of the foot fails, and the load “transfers” laterally, overwhelming the second metatarsal.
X-rays are the frontline imaging modality but require a high degree of clinical correlation.
Differential Diagnosis & Comparison
In a clinical setting, several conditions can mimic forefoot pain. It is the role of the Radiology Expert to distinguish these.
Comparison Summary Table
Feature | Metatarsal Stress Fracture | Morton’s Neuroma | Freiberg Infraction |
|---|---|---|---|
Primary Pain Site | Metatarsal Shaft (Dorsal) | Interdigital Space (Plantar) | Metatarsal Head (Joint) |
X-ray Finding | Callus/Periosteal Reaction | Normal | Head flattening/Sclerosis |
MRI Feature | Circumferential Bone Marrow Edema | Teardrop-shaped mass | Subchondral signal loss |
Clinical Test | Bone Percussion/Tuning Fork | Mulder’s Click | Joint Line Tenderness |
While callus formation on an X-ray is diagnostic, Advanced Imaging (MRI) is the “Gold Standard” for early detection or complex cases.
Chiropractic or Conservative Care
Allopathic/Medical Referral
Every day, chiropractors face the same frustration: imaging reports that miss what matters. General radiologists weren’t trained in your world; they don’t understand subluxations, joint dysfunction, or the biomechanical findings that drive your treatment decisions.
The result? Delayed care. Uncertain patients. Cases that stall when they should be progressing.
The Kinetic Radiology Difference: Chiropractors Reading for Chiropractors
Our board-certified DACBRs aren’t just radiologists. We’re chiropractors who chose to specialize in musculoskeletal imaging. We speak your language because we’ve stood where you stand.
Reports You Can Act On Immediately – No vague findings. No irrelevant details. Just the specific insights that guide your next adjustment, your treatment plan, and your patient conversations.
Same-Day Turnaround – Your patients don’t want to wait days wondering what’s wrong. Neither should you. Get clarity fast so care never stalls.
Documentation That Protects Your Practice – Whether it’s insurance requirements, legal protection, or patient records, our reports give you the clinical backing you need.
Confidence That Builds Your Reputation – When patients see you consulting with specialized radiologists, they recognize your commitment to excellence. That trust turns into loyalty, referrals, and five-star reviews.
Think about the last complex case you handled. Did the radiology report actually help you—or did you have to fill in the gaps yourself?
Now imagine having a DACBR partner who catches the subtle findings, flags the red flags, and gives you confidence in every diagnosis.
No commitment. No risk. Just submit your next challenging case and experience what specialized chiropractic radiology can do for your clinical confidence and patient outcomes.
Questions? Call us at 321 325 0096 or email at support@kineticradiology.com
Yes, initial X-rays are often negative in the first 2–3 weeks of symptoms.
Initial plain film radiography has a low sensitivity (15–35%) for acute stress fractures. Because these are “fatigue” injuries rather than acute traumatic breaks, the fracture line is often microscopic. It typically takes 14 to 21 days for the body to produce enough hazy callus formation or periosteal reaction to be visible on a standard Radiology Report. If clinical suspicion remains high despite a negative X-ray, a DACBR will often recommend MRI or a follow-up study.
It indicates the bone is in the process of healing a previous or ongoing stress injury.
Hazy callus formation is a hallmark radiographic sign of a subacute stress fracture. It represents the “woven bone” the body deposits to bridge a micro-fracture. In the context of the second metatarsal, this indicates the bone has reached its “fatigue” limit, and the osteoblastic activity is attempting to reinforce the cortex. Seeing this on an image confirms the diagnosis of a stress injury that has been present for at least several weeks.
Its rigid attachment to the cuneiforms makes it a primary weight-bearing lever that lacks flexibility.
Biomechanically, the second metatarsal is the longest and most “fixed” of the metatarsals, articulating deeply with the intermediate cuneiform. Unlike the first or fifth metatarsals, which have more mobility, the second acts as a rigid fulcrum during the “toe-off” phase of gait. When a runner increases volume, this bone absorbs the brunt of the force, leading to the microdamage seen by Radiology Experts.
Usually no, but it is used if the diagnosis is unclear or to rule out soft tissue injuries.
If the X-ray clearly shows a “gray cortex” sign or exuberant callus, an MRI may not be required for the diagnosis. However, Diagnostic Imaging Consultants often recommend MRI to assess the extent of bone marrow edema (BME) or to differentiate the pain from a Morton’s neuroma or plantar plate tear, which can coexist with bone stress.
Partnering with a DACBR teleradiology service provides more than just a second opinion; it offers a significant return on investment:
Speed: Get expert reports in hours, not days.
Expertise: Access board-certified specialists without having to hire them.
Convenience: The entire process is handled online from your office.
Clarity: Receive clear, concise reports that are clinically relevant to chiropractic care, not generic medical reports.
Posted onTrustindex verifies that the original source of the review is Google. Prompt efficient service that is thorough and clear. Spinal information is top notch and I've had patients discover kidney stones and possible issues with a hip joint replacement loosening as incidental findings that supported both me and the patient above expectations.Posted onTrustindex verifies that the original source of the review is Google. Quick, accurate, and easy to work with. My new radiology team!Posted onTrustindex verifies that the original source of the review is Google. Excellent, timely reads. Invaluable for CBCTPosted onTrustindex verifies that the original source of the review is Google. Best turnaround time and thorough reports out of any radiologist I’ve seen or worked with!Posted onTrustindex verifies that the original source of the review is Google. Very detailed reports and quick service. Highly recommendedPosted onTrustindex verifies that the original source of the review is Google. Fast turn around time for the radiology reports! Thank you for making this process as seamless as possible!Posted onTrustindex verifies that the original source of the review is Google. I am a NUCCA chiropractor located in Wauankee Wisconsin and I can tell you Dr. Rishi is the only radiologist I’d work with. Sure there are many others in my area but when you want the best you go to the best. He is very easy to work with and always fast to respond and report. 100% recommend.Posted onTrustindex verifies that the original source of the review is Google. Kinetic Radiology is great! They were able to read and get a report written immediately. They are my go to company for any and all images that I need read!Posted onTrustindex verifies that the original source of the review is Google. Working with Kinetic Radiology has been a fantastic experience. Their team is consistently timely in reading our imaging, which greatly enhances our workflow and patient care. The communication is clear and effective, making collaboration seamless. Every interaction with their staff has been professional and supportive, always ready to address any questions or concerns. Their commitment to excellence and efficiency sets them apart. I highly recommend Kinetic Radiology for anyone seeking reliable and responsive radiology services.Posted onTrustindex verifies that the original source of the review is Google. Our office in Northern Michigan was looking for a radiology interpretation service that we could occasionally get second opinions from for the X-rays we take in house. I had heard great things about Kinetic Radiology from a colleague, so I reached out and we decided to give their services a try. After going through the sign up process and now having received our first radiology report back, I have to say that I am so happy we chose the team at Kinetic Radiology. From the start they were so helpful and answered all of the questions my office and I had, they were timely in their back and forth communication with us, the entire process was seamless, and they provided us with a detailed and thorough radiology report faster than expected. If you are looking for an interpretation service for you our your office, I would definitely give the radiologists at Kinetic Radiology a try!Load more
We service all 50 U.S. States, including the following States and Cities listed below.
Copyright 2024 Kinetic Radiology All Rights Reserved
Website Privacy | Terms of UseReceive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.
Copyright 2024 Kinetic Radiology
All Rights Reserved
Receive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.