Paget Disease of Bone, also known as Osteitis Deformans, is a chronic skeletal disorder characterized by focal areas of abnormal bone remodeling affecting one or more skeletal sites. This condition represents the second most common metabolic bone disease after osteoporosis and results from excessive bone breakdown (resorption) followed by disorganized, exuberant bone formation that creates enlarged, weakened, and structurally abnormal bone. The newly formed pagetic bone is poorly organized, inadequately mineralized, and laid down in an irregular mosaic pattern rather than normal lamellar architecture. [ncbi.nlm.nih]
While many patients with Paget Disease remain asymptomatic throughout their lives, those who develop symptoms typically present with bone pain, skeletal deformities, and various complications including pathologic fractures, secondary osteoarthritis affecting adjacent joints, and neurological compromise from nerve compression. The disease has a strong predilection for the pelvis, spine, femur, tibia, and skull, though any bone can be affected. Early recognition through diagnostic imaging and appropriate referral to specialists or consultation with diagnostic imaging consultants can significantly improve patient outcomes and prevent serious complications.
For practitioners who encounter suspicious imaging findings, seeking a radiology second opinion from a board-certified DACBR (Diplomate of the American Chiropractic Board of Radiology) can provide valuable diagnostic clarity and ensure appropriate patient management strategies are implemented promptly.

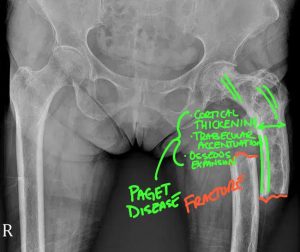
Pathological fracture of the left femur secondary to Paget disease. Paget disease has remodeled the osseous structure to demonstrate cortical thickening, trabecular accentuation, and osseous expansion. This weakened bone is now susceptible to a pathological fracture that will typically take on a transverse orientation.
Understanding the epidemiologic profile of Paget Disease helps practitioners maintain appropriate clinical suspicion when evaluating at-risk patients. The disease predominantly affects individuals over the age of 50 years, with prevalence increasing substantially with advancing age. Men are affected more frequently than women, with some studies suggesting a male-to-female ratio of approximately 3:2.
Geographic distribution shows remarkable variation, with the highest prevalence observed in England, Scotland, central Europe, Greece, Australia, and New Zealand, as well as countries settled by European immigrants including the United States and Canada. Conversely, the disease is uncommon in Scandinavia, Asia, Africa, and the Middle East. These geographic patterns suggest both genetic and potential environmental factors in disease pathogenesis.
Family history represents a significant risk factor, as up to 40% of patients with Paget Disease have affected first-degree relatives. Having a positive family history increases an individual’s risk 7- to 10-fold compared to the general population. Approximately 10% of patients harbor germline mutations in the SQSTM1 (sequestosome-1) gene, which results in increased nuclear factor kappa-B activity and enhanced osteoclast activity. Additional mutations affecting the RANK (receptor activator of nuclear factor kappa-B) signaling pathway, which is critical for osteoclast generation and function, have also been identified in association with Paget Disease.
Interestingly, epidemiologic studies have documented a declining incidence and severity of Paget Disease over the past 20-25 years in several countries. The reasons for this trend remain unclear but may involve changes in environmental factors or improved overall health and nutrition in affected populations.
The pathophysiology of Paget Disease involves a complex, dysregulated process of bone remodeling that unfolds in distinct stages. Understanding these mechanisms helps practitioners recognize the radiographic manifestations and clinical consequences of the disease.
The primary cellular abnormality in Paget Disease resides within osteoclasts, the cells responsible for bone resorption. Pagetic osteoclasts demonstrate a characteristic “pagetic phenotype” with increased osteoclast number and size, increased nuclei per osteoclast (often containing 10-100 nuclei compared to 3-5 in normal osteoclasts), and increased responsiveness to osteoclast-inducing factors. These abnormal osteoclasts exhibit enhanced bone resorption capacity, creating focal areas of intense bone breakdown.
The disease progresses through four pathological stages:
Stage 1 (Osteolytic/Lytic Phase): Characterized by predominant osteoclastic activity with increased bone resorption, leading to decreased bone mass and lytic lesions. This stage represents the early, active phase of the disease.
Stage 2 (Mixed Phase): Features both osteoclastic and osteoblastic activity occurring simultaneously. The excessive bone resorption triggers a compensatory osteoblastic response through a sensing mechanism that detects bone loss.
Stage 3 (Osteoblastic/Sclerotic Phase): Dominated by osteoblastic activity with new bone formation. The pagetic osteoclasts express increased levels of coupling factors that drive aberrant, excessive bone formation. Despite this increased bone formation, the newly created bone is structurally disorganized, poorly mineralized, and mechanically weak.
Stage 4 (Malignant Degeneration): In rare cases (less than 1% of patients), malignant transformation to osteosarcoma or other bone sarcomas may occur.
The excessive, disorganized bone formation in Paget Disease results in weak woven bone with collagen fibers laid down in an irregular mosaic pattern rather than the normal parallel lamellar arrangement. Pagetic bone is highly vascularized and demonstrates intense metabolic activity, yet despite increased size, it has poor biomechanical efficiency due to its structural disorganization. These features result in various clinical consequences including bone deformities, increased fracture risk, nerve compression from bone expansion, and secondary osteoarthritis from abnormal joint loading.
When diagnostic imaging consultants or a DACBR evaluate radiographs showing these pathophysiologic changes, they can correlate the imaging appearances with the underlying disease stage and provide crucial guidance regarding disease activity and progression.
The clinical presentation of Paget Disease varies considerably, ranging from completely asymptomatic cases discovered incidentally to severely symptomatic patients with multiple complications. Understanding the spectrum of presentations enables practitioners to maintain appropriate clinical suspicion and initiate timely diagnostic evaluation.
Asymptomatic Presentation
The majority of patients with Paget Disease—estimates suggest 70-90%—remain asymptomatic throughout their lives. These cases are typically discovered incidentally through one of three mechanisms: radiographs obtained for unrelated reasons showing characteristic bone changes, routine laboratory testing revealing unexplained elevated serum alkaline phosphatase levels, or bone scans performed for other indications demonstrating increased radiotracer uptake in affected bones. When asymptomatic cases are identified, consultation with diagnostic imaging consultants or obtaining a radiology second opinion from a DACBR can help confirm the diagnosis and guide monitoring strategies.
Symptomatic Presentation
When symptoms do occur, bone pain represents the most common complaint. The pain associated with Paget Disease typically exhibits characteristic features that help distinguish it from other musculoskeletal conditions. Patients describe the pain as dull or aching in quality, localized deep within the affected bone, constant rather than intermittent, and notably worse at night. Physical examination may reveal warmth over the affected bone due to increased vascularity.
The specific clinical manifestations depend heavily on which skeletal sites are involved:
Pelvic Involvement: The pelvis is the most commonly affected site, involved in 30-75% of cases. Patients may experience hip pain arising either from direct bone involvement or from secondary osteoarthritis developing in the hip joint as a consequence of altered biomechanics and abnormal joint loading. Gait disturbances may develop due to pain, deformity, or leg-length discrepancy.
Spinal Involvement: Vertebral Paget Disease affects 30-75% of patients and can produce diverse symptoms. Nerve root compression from vertebral expansion, spinal stenosis, or pathologic fracture can cause radiculopathy with pain, tingling, numbness, and weakness radiating into the extremities. In severe cases, spinal cord compression may occur, representing a surgical emergency. The characteristic “picture frame” vertebra appearance on radiographs often prompts practitioners to seek a radiology second opinion to confirm the diagnosis.
Skull Involvement: Affecting 25-65% of cases, skull involvement can produce headaches, hearing loss (from temporal bone involvement affecting the ossicles or compression of the eighth cranial nerve), vertigo, tinnitus, and rarely cranial nerve palsies. Skull enlargement may be noticeable, with patients reporting that hats no longer fit properly.
Long Bone Involvement: The femur and tibia are commonly affected, with involvement occurring in 25-35% and 30-55% of cases respectively. Long bone disease can produce visible and palpable bone enlargement, characteristic bowing deformities (particularly anterior-lateral bowing of the femur or anterior bowing of the tibia creating a bowlegged appearance), increased susceptibility to pathologic fractures (often transverse “chalk-stick” fractures through sclerotic bone), and secondary osteoarthritis in adjacent joints such as the knee or hip.
Complications Requiring Urgent Evaluation
Certain presentations warrant immediate medical evaluation and referral. Red flag symptoms that should prompt urgent assessment include partial loss of limb movement suggesting nerve compression or spinal cord involvement, loss of bowel or bladder control indicating cauda equina syndrome or spinal cord compression, sudden severe pain suggesting pathologic fracture, and rapidly progressive pain that may indicate malignant transformation. When these complications are suspected on imaging, immediate consultation with diagnostic imaging consultants or a DACBR specializing in musculoskeletal radiology can expedite appropriate referral and management.
Diagnostic imaging plays a central role in establishing the diagnosis of Paget Disease, determining disease extent, monitoring progression, and identifying complications. Understanding the characteristic imaging features across different modalities enables accurate diagnosis and appropriate patient management.
Radiography (Plain Films)
Plain radiography remains the cornerstone imaging modality for diagnosing Paget Disease and represents the initial examination of choice when the condition is suspected. The radiographic manifestations vary according to the pathologic stage of disease.
Lytic (Early) Phase: The early osteolytic phase demonstrates intense osteoclastic activity manifesting as areas of bone lysis and rarefaction. In the skull, this appears as well-defined geographic areas of radiolucency termed osteoporosis circumscripta. In long bones, the lytic phase produces a characteristic wedge-shaped or V-shaped area of radiolucency that advances through the bone with a sharply demarcated margin, described as having a “flame-shaped” or “blade of grass” configuration. This advancing front of osteolysis typically extends from the metaphysis toward the diaphysis and represents one of the most pathognomonic features of Paget Disease.
Mixed Phase: As the disease progresses, radiographs demonstrate combined lytic and sclerotic changes reflecting simultaneous bone resorption and formation. This transitional phase shows a mixture of radiolucent and radiodense areas within affected bones.
Sclerotic (Late) Phase: The late sclerotic phase features predominant bone formation and produces the most recognizable radiographic manifestations of Paget Disease. Characteristic findings include trabecular coarsening and distortion creating a “cotton wool” appearance particularly in the skull, marked cortical thickening that may be disproportionate to the degree of sclerosis, bone enlargement (hypertrophy) with expansion of the normal bone contour, the pathognomonic “picture frame” appearance in vertebrae (peripheral sclerosis with relatively lucent central portion), and increased bone density that may be uniform or heterogeneous.
Additional radiographic features that support the diagnosis include involvement extending to the articular surface (epiphyseal involvement), sharply demarcated advancing front of osteolysis, widespread osteosclerosis, bony enlargement, coarsened trabecular pattern, and bone deformity such as bowing of long bones or basilar invagination of the skull.
When chiropractors, primary care providers, or urgent care physicians encounter these characteristic radiographic findings, consultation with diagnostic imaging consultants or requesting a radiology second opinion from a DACBR ensures accurate interpretation and appropriate follow-up recommendations. A board-certified DACBR possesses specialized training in recognizing the spectrum of Paget Disease manifestations and differentiating them from mimicking conditions.
Bone Scintigraphy (Bone Scan)
Radionuclide bone scintigraphy using technetium-99m bisphosphonate compounds is recommended for delineating the full extent of metabolically active disease throughout the skeleton. Affected bones demonstrate intense radiotracer uptake that is typically more pronounced than in most other bone pathologies, reflecting the marked increase in bone turnover. Bone scintigraphy is particularly valuable for identifying clinically silent sites of involvement, determining whether disease is monostotic (single bone) or polyostotic (multiple bones), and establishing a baseline for monitoring disease progression or treatment response. Once polyostotic disease is identified, plain radiographs of all metabolically active sites should be obtained for detailed characterization.
Computed Tomography (CT)
While not typically used for initial diagnosis, CT provides superior depiction of the altered bone architecture compared to plain radiography. CT clearly demonstrates coarsened, thickened trabeculae, cortical thickening and expansion, bone hypertrophy, and the degree of skeletal deformity. CT is particularly valuable for evaluating complications including pathologic fractures, the extent of spinal stenosis and nerve compression, malignant transformation (suggested by cortical destruction and soft tissue mass), and basilar invagination in skull involvement. When complex cases require detailed anatomic assessment, diagnostic imaging consultants may recommend CT as an adjunct to radiography.
Magnetic Resonance Imaging (MRI)
MRI demonstrates variable signal characteristics depending on the balance between marrow replacement, sclerosis, and residual fatty marrow. Common MRI findings include mixed patterns of increased and decreased T1 signal within affected bones, band-like areas of decreased T1 and T2 signal at vertebral endplates, vertebral body expansion, and variable enhancement after gadolinium administration. MRI excels at evaluating marrow characteristics, assessing soft tissue complications such as nerve compression or spinal stenosis, differentiating Paget Disease from metastatic disease in ambiguous cases, and detecting sarcomatous transformation. However, MRI does not depict bone mineralization and trabecular architecture as clearly as radiography or CT, limiting its utility for initial diagnosis.
When imaging findings are atypical or raise concern for alternative diagnoses or complications, obtaining a radiology second opinion from an experienced DACBR can provide valuable diagnostic insight and guide subsequent management decisions.
Chiropractors, primary care physicians, and urgent care practitioners play critical roles in the detection, appropriate referral, and co-management of patients with Paget Disease. Understanding these responsibilities ensures optimal patient outcomes.
Early Detection and Recognition
Many cases of Paget Disease are first identified by chiropractors or primary care providers who order radiographs for musculoskeletal complaints or obtain laboratory tests showing unexplained alkaline phosphatase elevation. Recognizing the characteristic radiographic features—bone expansion, cortical thickening, trabecular coarsening, mixed lytic-sclerotic changes, and the pathognomonic advancing “flame” or “blade of grass” lytic front—enables early diagnosis before complications develop.
When characteristic imaging findings are encountered, chiropractors and other practitioners should consider consultation with diagnostic imaging consultants or obtaining a radiology second opinion from a board-certified DACBR to confirm the diagnosis and receive guidance regarding disease extent, activity, and need for additional imaging or laboratory evaluation. A DACBR possesses specialized training in recognizing Paget Disease across its various stages and anatomic distributions, ensuring accurate diagnosis and appropriate recommendations.
Clinical Assessment
Practitioners should conduct thorough symptom assessment when Paget Disease is suspected or confirmed, evaluating bone pain patterns, neurologic symptoms suggesting nerve compression, hearing changes in patients with skull involvement, and signs of deformity or gait disturbance. Physical examination should assess for bone tenderness, warmth over affected areas, visible or palpable bone enlargement, skeletal deformities, and neurologic deficits.
Appropriate Referral
Timely referral to specialists ensures patients receive appropriate disease-specific treatment and monitoring. Referral to rheumatology, endocrinology, or metabolic bone specialists is indicated for confirmed or highly suspected Paget Disease requiring treatment initiation and management, disease activity assessment and monitoring, and complex cases with extensive involvement or complications.
Immediate referral is warranted for red flag presentations including suspected pathologic fracture, new-onset neurological deficits such as bowel/bladder dysfunction, progressive weakness, or severe radiculopathy, rapidly progressive bone pain suggesting possible malignant transformation, and hearing loss or cranial nerve symptoms requiring urgent evaluation.
Co-Management Considerations
For patients with confirmed Paget Disease under specialist care, chiropractors and primary care providers can contribute to comprehensive management through monitoring for new symptoms or complications, reinforcing medication adherence and follow-up recommendations, managing comorbid conditions and musculoskeletal complaints, and coordinating care between specialists.
However, practitioners must recognize important treatment contraindications and modifications. Paget Disease represents a relative to absolute contraindication for high-velocity, low-amplitude (HVLA) spinal manipulation directly over affected bones due to substantially increased fracture risk. Bone weakening and destructive disorders, including Paget Disease, are specifically identified as contraindications requiring treatment modification in chiropractic clinical practice guidelines.
When managing patients with Paget Disease, chiropractors should avoid HVLA manipulation of affected vertebrae or long bones, consider alternative manual techniques including soft tissue therapy, mobilization, and instrument-assisted manipulation that avoid high-force thrusts, and focus therapeutic interventions on addressing secondary complications such as adjacent joint dysfunction, muscle imbalances, and postural adaptations.
Conservative care for associated musculoskeletal complaints may include soft tissue therapies targeting muscle tension and compensatory patterns, therapeutic exercise for maintaining strength and mobility, postural education and ergonomic counseling, and management of secondary osteoarthritis in adjacent joints through appropriate modalities and lifestyle modifications. All conservative interventions should be tailored to avoid high-force techniques over fragile pagetic bone while addressing patient symptoms and functional limitations.
Obtaining Expert Imaging Consultation
When radiographic findings suggest Paget Disease or when imaging features are atypical, obtaining consultation with diagnostic imaging consultants or requesting a radiology second opinion from a DACBR provides significant value. Board-certified DACBRs possess specialized postgraduate training in diagnostic imaging interpretation, including advanced education in recognizing metabolic bone diseases, skeletal pathology, and complex musculoskeletal conditions.
A radiology second opinion from an experienced DACBR can confirm or refute the suspected diagnosis, differentiate Paget Disease from mimicking conditions, assess disease extent and activity, identify complications such as fractures or malignant transformation, and provide evidence-based recommendations for additional imaging or specialist referral. This consultation enhances diagnostic confidence and ensures appropriate patient management, ultimately improving outcomes and preventing complications.
Many diagnostic imaging consultants and DACBR services offer teleradiology consultation, making expert subspecialty imaging interpretation accessible to practitioners regardless of geographic location. These services can be particularly valuable for chiropractors who regularly interpret radiographs and wish to ensure diagnostic accuracy for complex or unusual findings.
Every day, chiropractors face the same frustration: imaging reports that miss what matters. General radiologists weren’t trained in your world; they don’t understand subluxations, joint dysfunction, or the biomechanical findings that drive your treatment decisions.
The result? Delayed care. Uncertain patients. Cases that stall when they should be progressing.
The Kinetic Radiology Difference: Chiropractors Reading for Chiropractors
Our board-certified DACBRs aren’t just radiologists. We’re chiropractors who chose to specialize in musculoskeletal imaging. We speak your language because we’ve stood where you stand.
Reports You Can Act On Immediately – No vague findings. No irrelevant details. Just the specific insights that guide your next adjustment, your treatment plan, and your patient conversations.
Same-Day Turnaround – Your patients don’t want to wait days wondering what’s wrong. Neither should you. Get clarity fast so care never stalls.
Documentation That Protects Your Practice – Whether it’s insurance requirements, legal protection, or patient records, our reports give you the clinical backing you need.
Confidence That Builds Your Reputation – When patients see you consulting with specialized radiologists, they recognize your commitment to excellence. That trust turns into loyalty, referrals, and five-star reviews.
Think about the last complex case you handled. Did the radiology report actually help you—or did you have to fill in the gaps yourself?
Now imagine having a DACBR partner who catches the subtle findings, flags the red flags, and gives you confidence in every diagnosis.
No commitment. No risk. Just submit your next challenging case and experience what specialized chiropractic radiology can do for your clinical confidence and patient outcomes.
Questions? Call us at 321 325 0096 or email at support@kineticradiology.com
Paget Disease of Bone is a chronic disorder causing abnormal bone remodeling that results in enlarged, weakened bones that are structurally disorganized. [mayoclinic]
Paget Disease of Bone, also called Osteitis Deformans, is a metabolic bone disorder characterized by excessive bone breakdown followed by disorganized bone formation. The disease disrupts the body’s normal bone recycling process, where old bone tissue is replaced by new bone. In Paget Disease, overactive osteoclasts break down bone tissue too rapidly, triggering excessive compensatory bone formation that creates poorly organized, weakened bone despite appearing enlarged or thickened on imaging. When chiropractors or primary care providers identify suspicious findings on radiographs, consultation with diagnostic imaging consultants or obtaining a radiology second opinion from a DACBR can confirm the diagnosis and provide guidance on disease extent and management. The condition most commonly affects the pelvis, spine, femur, tibia, and skull, though any bone can be involved. [niams.nih]
Paget Disease is not contagious but has a strong hereditary component, with 15-30% of cases showing familial inheritance patterns. [medlineplus]
Paget Disease cannot be transmitted from person to person—it is not an infectious or contagious condition. However, genetics play a significant role in disease development. Approximately 40% of patients with Paget Disease have affected first-degree relatives, and having a family history increases risk 7- to 10-fold. In familial cases, the disease follows an autosomal dominant inheritance pattern with incomplete penetrance, meaning that inheriting the gene mutation doesn’t guarantee disease development. Mutations in the SQSTM1 gene are found in 40-50% of inherited cases and 10-15% of sporadic cases without family history. Additional genes including RANK and regions on chromosomes 5, 6, and 18 have been linked to the disease. When radiographic findings suggest Paget Disease in patients with positive family history, diagnostic imaging consultants or a DACBR can provide expert interpretation and recommend appropriate genetic counseling if indicated. [sciencedirect]
Paget Disease is diagnosed through a combination of characteristic radiographic findings and elevated serum alkaline phosphatase levels. [mayoclinic]
Diagnosis typically involves multiple components. Plain radiographs (X-rays) remain the primary diagnostic tool, showing characteristic features including bone enlargement, cortical thickening, coarsened trabeculae, mixed lytic-sclerotic changes, and the pathognomonic “flame-shaped” or “blade of grass” advancing lytic front in long bones. Blood tests revealing elevated serum alkaline phosphatase (ALP) support the diagnosis and reflect increased bone turnover activity. However, elevated ALP can occur in other conditions, so imaging correlation is essential. Bone scans using radioactive tracers help determine disease extent by identifying all metabolically active skeletal sites. Physical examination may reveal bone enlargement, warmth over affected areas, or deformities. When imaging findings are subtle or atypical, obtaining a radiology second opinion from a board-certified DACBR ensures accurate diagnosis. Diagnostic imaging consultants with specialized training in metabolic bone disorders can differentiate Paget Disease from conditions like metastatic disease, fibrous dysplasia, or osteosarcoma that may appear similar on initial imaging. [arthritis-uk]
Paget Disease cannot be cured, but it can be effectively controlled with bisphosphonate medications that provide prolonged remission periods. [aafp]
While there is no cure for Paget Disease, modern treatments can successfully control the disorder and significantly improve quality of life. Bisphosphonate medications—the primary treatment—work by inhibiting excessive osteoclast activity and regulating abnormal bone remodeling. Treatment with bisphosphonates like zoledronic acid can normalize bone turnover markers and provide prolonged remission lasting months or years after treatment completion. When started before major complications develop, treatment is highly effective at eliminating or reducing bone pain, preventing progression of deformities, reducing fracture risk, and preventing neurological complications. The goal of treatment is disease control rather than cure—slowing excessive bone turnover and inducing remission to prevent complications. Regular monitoring with alkaline phosphatase measurements and periodic imaging helps assess treatment response. Chiropractors and primary care providers managing patients with Paget Disease should coordinate with specialists and may benefit from consultation with diagnostic imaging consultants or a DACBR to monitor disease progression and identify complications requiring treatment modification. [paget.org]
Partnering with a DACBR teleradiology service provides more than just a second opinion; it offers a significant return on investment:
Speed: Get expert reports in hours, not days.
Expertise: Access board-certified specialists without having to hire them.
Convenience: The entire process is handled online from your office.
Clarity: Receive clear, concise reports that are clinically relevant to chiropractic care, not generic medical reports.
Posted onTrustindex verifies that the original source of the review is Google. Prompt efficient service that is thorough and clear. Spinal information is top notch and I've had patients discover kidney stones and possible issues with a hip joint replacement loosening as incidental findings that supported both me and the patient above expectations.Posted onTrustindex verifies that the original source of the review is Google. Quick, accurate, and easy to work with. My new radiology team!Posted onTrustindex verifies that the original source of the review is Google. Excellent, timely reads. Invaluable for CBCTPosted onTrustindex verifies that the original source of the review is Google. Best turnaround time and thorough reports out of any radiologist I’ve seen or worked with!Posted onTrustindex verifies that the original source of the review is Google. Very detailed reports and quick service. Highly recommendedPosted onTrustindex verifies that the original source of the review is Google. Fast turn around time for the radiology reports! Thank you for making this process as seamless as possible!Posted onTrustindex verifies that the original source of the review is Google. I am a NUCCA chiropractor located in Wauankee Wisconsin and I can tell you Dr. Rishi is the only radiologist I’d work with. Sure there are many others in my area but when you want the best you go to the best. He is very easy to work with and always fast to respond and report. 100% recommend.Posted onTrustindex verifies that the original source of the review is Google. Kinetic Radiology is great! They were able to read and get a report written immediately. They are my go to company for any and all images that I need read!Posted onTrustindex verifies that the original source of the review is Google. Working with Kinetic Radiology has been a fantastic experience. Their team is consistently timely in reading our imaging, which greatly enhances our workflow and patient care. The communication is clear and effective, making collaboration seamless. Every interaction with their staff has been professional and supportive, always ready to address any questions or concerns. Their commitment to excellence and efficiency sets them apart. I highly recommend Kinetic Radiology for anyone seeking reliable and responsive radiology services.Posted onTrustindex verifies that the original source of the review is Google. Our office in Northern Michigan was looking for a radiology interpretation service that we could occasionally get second opinions from for the X-rays we take in house. I had heard great things about Kinetic Radiology from a colleague, so I reached out and we decided to give their services a try. After going through the sign up process and now having received our first radiology report back, I have to say that I am so happy we chose the team at Kinetic Radiology. From the start they were so helpful and answered all of the questions my office and I had, they were timely in their back and forth communication with us, the entire process was seamless, and they provided us with a detailed and thorough radiology report faster than expected. If you are looking for an interpretation service for you our your office, I would definitely give the radiologists at Kinetic Radiology a try!Load more
We service all 50 U.S. States, including the following States and Cities listed below.
Copyright 2024 Kinetic Radiology All Rights Reserved
Website Privacy | Terms of UseReceive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.
Copyright 2024 Kinetic Radiology
All Rights Reserved
Receive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.