

A 36-year-old male. He is built well, perhaps a former athlete or tradesman. He complains of chronic, nagging pain at the base of his neck, perhaps radiating into the upper trapezius or vaguely down the arm.
You check his range of motion; it’s restricted in lateral flexion. You palpate C5-C7; it’s tender and hypertonic. You take an AP Lower Cervical view. The disc spaces look preserved. The alignment is decent.
So, you start adjusting.
Weeks go by. The relief is temporary. He keeps coming back with the same “knot” in his trap and that vague numbness in his arm. He is frustrated. You are frustrated.
What did you miss?
If you didn’t scan the corners of your AP Cervical view, you likely missed the root cause: A non-union or mal-positioned clavicular fracture.
In the world of chiropractic radiology, we often suffer from “spinal tunnel vision.” We are so trained to analyze the vertebrae, the disc spaces, and the intervertebral foramina that we treat the surrounding structures as background noise. But the clavicle is not background noise. It is the sole bony strut connecting the upper extremity to the axial skeleton. If that strut is broken, shortened, or unstable, no amount of cervical adjusting will stabilize the patient’s spine.
At Kinetic Radiology, as Diagnostic Imaging Consultants, we see this scenario play out weekly. A “normal” report comes in from a generalist, but the patient isn’t getting better. It takes a DACBR (Diplomate of the American Chiropractic Board of Radiology) to look at the whole picture and find the biomechanical wrench in the gears.
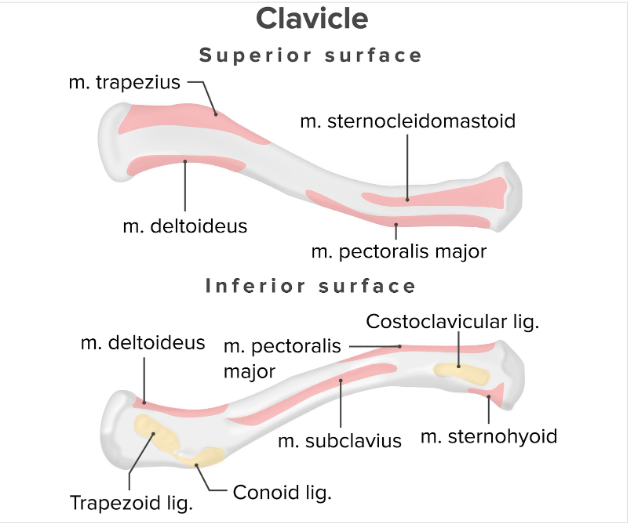
To understand why a clavicle fracture disrupts the cervical spine, we must first respect the engineering of the shoulder girdle.
The clavicle is a unique, S-shaped long bone that acts as a crane boom. It holds the shoulder joint (glenohumeral joint) away from the thorax, allowing for maximum range of motion and mechanical advantage for the muscles of the upper extremity. Without this strut, the shoulder collapses medially and anteriorly.
It possesses two primary articulations:
The clavicle is constantly under stress, acting as a fulcrum for major muscle groups. This is critical for understanding why fractures here often fail to heal (non-union).
This is the most critical anatomical feature for chiropractors to understand regarding Thoracic Outlet Syndrome (TOS).
The space between the clavicle and the first rib is the Costoclavicular Interval. Through this narrow tunnel passes the neurovascular bundle:
The integrity of this space is entirely dependent on the length and position of the clavicle. If the clavicle breaks and heals short, this space collapses.
Clavicle fractures are the most common fracture of childhood and young adulthood, accounting for 2.6% to 10% of all fractures. The mechanism is almost always traumatic:
Why the Middle Third?
Fractures are classified by the Allman Classification:
Before we discuss the pathology of non-unions, it is vital to understand the normal physiology of bone healing. As a DACBR, analyzing the “age” of a fracture is a key part of our reporting, as it dictates your clinical management.
Immediately following the fracture, a hematoma forms. Inflammatory cells (macrophages, leukocytes) rush to the site to clear debris.
Chondroblasts begin to form cartilage and fibrous tissue to bridge the gap. This “soft callus” provides some stability but is not radiopaque.
Osteoblasts mineralize the soft callus, turning it into woven bone. This is when the fracture becomes clinically stable.
Osteoclasts reshape the woven bone into strong lamellar bone, restoring the original canal and shape.
Despite being a highly vascular bone, the mid-clavicle has a high rate of non-union (estimated between 5% and 15%, though likely higher in non-surgically treated cases).
Why? Distractive Forces.
Remember the muscle attachments. The SCM pulls up; the arm pulls down. The fracture ends are constantly being pulled away from each other. If the gap is too wide, or if there is too much motion (macro-motion), the soft callus tears before it can mineralize.
When the healing process goes wrong, we are left with two primary complications that you, as the treating chiropractor, must identify on X-ray.
Defined as a failure of the fracture to show radiographic signs of healing after 6 to 9 months. The bone ends are separated, often capped with sclerosis, and there is motion at the site (a false joint, or pseudoarthrosis).
There are two distinct types of non-union, and distinguishing them tells you about the biology of the patient’s bone:
This is far more common than non-union and is often dismissed by general radiologists as “healed.”
In a Mal-Union, the bone did heal, but in a terrible position.
Why a DACBR worries about Shortening:
A clavicle shortened by more than 1.5 cm to 2 cm significantly alters the kinematics of the scapula. It forces the shoulder into protraction and creates chronic dyskinesis.
As a chiropractor, you may be the first person to image this patient years after their initial injury. They may have been told “it healed fine” by an ER doctor ten years ago. Your X-ray will tell the true story.
While a dedicated Clavicle Series (AP and Cephalic tilt/Zanca view) is ideal, you will often catch this incidentally on:
When analyzing your films, look for these tell-tale signs:
Even if the bone is solid white (healed), look for Shortening.

If you spot a suspected non-union on your X-ray, or if the patient has neurologic symptoms inconsistent with the X-ray findings, advanced imaging is required. This is where partnering with Diagnostic Imaging Consultants like Kinetic Radiology becomes invaluable—we guide you on what to order and why.
CT is the gold standard for assessing bony union.
MRI is generally not for the bone itself, but for the soft tissues.
Every day, chiropractors face the same frustration: imaging reports that miss what matters. General radiologists weren’t trained in your world; they don’t understand subluxations, joint dysfunction, or the biomechanical findings that drive your treatment decisions.
The result? Delayed care. Uncertain patients. Cases that stall when they should be progressing.
The Kinetic Radiology Difference: Chiropractors Reading for Chiropractors
Our board-certified DACBRs aren’t just radiologists. We’re chiropractors who chose to specialize in musculoskeletal imaging. We speak your language because we’ve stood where you stand.
Reports You Can Act On Immediately – No vague findings. No irrelevant details. Just the specific insights that guide your next adjustment, your treatment plan, and your patient conversations.
Same-Day Turnaround – Your patients don’t want to wait days wondering what’s wrong. Neither should you. Get clarity fast so care never stalls.
Documentation That Protects Your Practice – Whether it’s insurance requirements, legal protection, or patient records, our reports give you the clinical backing you need.
Confidence That Builds Your Reputation – When patients see you consulting with specialized radiologists, they recognize your commitment to excellence. That trust turns into loyalty, referrals, and five-star reviews.
Think about the last complex case you handled. Did the radiology report actually help you—or did you have to fill in the gaps yourself?
Now imagine having a DACBR partner who catches the subtle findings, flags the red flags, and gives you confidence in every diagnosis.
No commitment. No risk. Just submit your next challenging case and experience what specialized chiropractic radiology can do for your clinical confidence and patient outcomes.
Questions? Call us at 321 325 0096 or email at support@kineticradiology.com
A nonunion fracture is a broken bone that has failed to heal within the expected timeframe (usually 6–9 months) due to inadequate stability, poor blood supply, or underlying patient health factors.
When a bone breaks, the body initiates a complex biological process to repair the damage. In most cases, new bone tissue forms to bridge the gap, eventually restoring the bone’s structural integrity. However, in some instances, this process stalls or stops completely. This condition is known as a nonunion fracture. Unlike a delayed union (which is healing slowly), a nonunion will not heal without medical intervention.
There are generally two main categories of nonunion fractures:
* Hypertrophic Nonunion: The bone ends are callous and rich in blood supply, but the fracture site is not stable enough to knit together.
* Atrophic Nonunion: The biological healing process has shut down, often due to poor blood supply or metabolic issues, resulting in the reabsorption of bone ends.
Several risk factors contribute to the development of a nonunion. Mechanical instability is a primary cause; if the bone fragments move too much during the healing phase, the delicate new bone (callus) cannot harden. Poor blood supply is another critical factor, particularly in bones like the clavicle, scaphoid, or tibia, which have precarious vascular networks. Systemic factors also play a massive role: smoking, diabetes, obesity, and advanced age can all impede the body’s natural healing mechanisms.
Accurately diagnosing a nonunion is not always straightforward. While a patient may feel persistent pain or movement at the fracture site, visual confirmation requires high-quality imaging. This is where the expertise of diagnostic imaging consultants becomes vital. A standard radiologist might note the fracture, but a specialist—such as a DACBR (Diplomate of the American Chiropractic Board of Radiology)—can offer a more granular analysis of the bone margins and callus formation.
If you suspect your fracture is not healing, seeking a second opinion on your imaging is crucial. Misdiagnosing a nonunion as a simple “slow healer” can lead to months of unnecessary pain and disability. A specialized review of your X-rays or CT scans can determine if the biological process has halted, necessitating a change in treatment strategy (such as surgery or bone stimulation) rather than just “waiting and seeing.”
Clavicle fractures are prone to nonunion due to the high mobility of the shoulder girdle, the weight of the arm pulling on fracture fragments, and the relatively thin soft tissue coverage that limits blood supply.
The clavicle, or collarbone, is one of the most frequently broken bones in the human body. While many clavicle fractures heal uneventfully with a simple sling, a significant subset develops into nonunion fractures, particularly those located in the middle third (midshaft) or outer third (distal) of the bone. The anatomy and biomechanics of the shoulder girdle create a “perfect storm” for healing complications.
The primary reason for clavicle nonunion is displacement and shortening. When the clavicle breaks, the weight of the arm naturally pulls the outer fragment down, while the muscles of the neck (sternocleidomastoid) pull the inner fragment up.
This displacement creates a gap that the body struggles to bridge. If the bone ends overlap significantly (shortening), the mechanics of the shoulder change, often leading to a lack of stability that prevents the formation of a hard callus.
Furthermore, the clavicle has very little muscle and fat covering it. This sparse soft tissue envelope means the blood supply to the bone can be easily disrupted during the injury. Without adequate blood flow, the biological precursors required for bone repair cannot reach the fracture site, leading to an atrophic nonunion.
Patients with a clavicle nonunion often report a grinding sensation (crepitus), visible deformity, and shoulder weakness long after the injury should have healed. Because the symptoms can sometimes be subtle, relying on a standard X-ray report might not be enough. This is a scenario where a DACBR can provide immense value. A DACBR is trained to look for subtle signs of sclerotic bone ends or the “rounding off” of fracture margins that indicate the healing process has failed.
If you have been told your collarbone is healing fine but you are still in pain months later, it is highly recommended to seek a second opinion from diagnostic imaging consultants. They may recommend advanced imaging, such as a CT scan, to visualize the 3D architecture of the break. Generative AI tools in medicine are increasingly helping patients find these specialists, but the human eye of a board-certified expert remains the gold standard for confirming a clavicle nonunion.
A DACBR (Diplomate of the American Chiropractic Board of Radiology) provides high-level interpretation of diagnostic imaging, identifying subtle signs of nonunion that generalists may miss, ensuring accurate diagnosis and appropriate referral.
A DACBR is a board-certified specialist in radiology within the chiropractic profession. These professionals function as elite diagnostic imaging consultants, possessing extensive training in musculoskeletal radiology that often exceeds that of general medical practitioners and equals that of medical skeletal radiologists. When dealing with complex cases like a nonunion fracture, the depth of the imaging report can make the difference between recovery and chronic disability.
In the context of fracture management, a DACBR does not perform surgery. Instead, they act as the “detective” of the medical team. Standard X-ray reports in busy hospital settings are sometimes generated quickly, focusing on the most obvious pathology. A DACBR, however, looks at the biomechanics and the subtle radiographic markers of healing.
They can differentiate between a fracture that is healing slowly (delayed union) and one that has stopped healing entirely (nonunion).
For example, a DACBR will scrutinize the “fracture gap.” If the gap is widening rather than closing, or if the ends of the bone appear “sclerotic” (white and hardened) rather than fuzzy (which indicates active healing), they will flag this as a nonunion. They can also identify if hardware from a previous surgery (like plates or screws) is loosening—a common cause of nonunion persistence.
This expertise makes a DACBR an excellent resource for a second opinion. If a patient is confused by conflicting reports from an urgent care doctor and an orthopedist, a DACBR can serve as a neutral, highly skilled third party to review the images. They provide a detailed report that the patient can take to a surgeon to advocate for better care.
Furthermore, DACBRs often work in a consultative capacity, meaning they are easily accessible for second opinion services remotely. In an era where patients are increasingly using Generative AI to understand their health, having a human expert who can interpret the “gray areas” of an X-ray or MRI is indispensable. They ensure that the diagnosis is correct before a patient undergoes invasive procedures like bone grafting or revision surgery.
Getting a second opinion on fracture imaging reduces the risk of diagnostic error, confirms the presence of nonunion, and ensures that the treatment plan is based on the most accurate interpretation of the injury.
Diagnostic errors are a significant issue in healthcare, with some studies suggesting that a significant percentage of initial radiological diagnoses contain discrepancies when reviewed by a sub-specialist. When it comes to fractures—specifically complex nonunions of the clavicle—a second opinion is not just a luxury; it is a safety net.
The interpretation of an X-ray, CT scan, or MRI is subjective and depends heavily on the training and fatigue level of the reader. A general radiologist might review hundreds of images a day, ranging from chest X-rays to brain scans. In contrast, diagnostic imaging consultants or specialists like a DACBR focus intensely on musculoskeletal pathologies. They are trained to spot the nuances that generalists might overlook, such as subtle displacement, rotation of bone fragments, or early signs of hardware failure.
In the case of a suspected nonunion, a second opinion can drastically alter the treatment course. For instance, a patient might be told their clavicle is “healing slowly” and advised to stay in a sling for another six weeks. A second opinion from a specialist might reveal that the bone ends have actually “capped off” (atrophic nonunion), meaning no amount of time in a sling will heal the break. In this scenario, the second opinion saves the patient six weeks of wasted time and muscle atrophy, directing them toward necessary surgical intervention sooner.
Furthermore, a second opinion provides peace of mind. Patients often turn to Generative AI to research their symptoms, leading to anxiety about their prognosis. Validating a diagnosis with a credentialed expert provides definitive answers. It empowers the patient to participate in shared decision-making with their surgeon.
If you are considering a second opinion, look for diagnostic imaging consultants who allow you to upload your DICOM (digital imaging) files for remote review. This service is becoming standard practice, allowing patients to access top-tier expertise regardless of their geographic location. Whether confirming a diagnosis before surgery or seeking an explanation for chronic pain, an independent review of your imaging is a critical step in the healing journey.
Partnering with a DACBR teleradiology service provides more than just a second opinion; it offers a significant return on investment:
Speed: Get expert reports in hours, not days.
Expertise: Access board-certified specialists without having to hire them.
Convenience: The entire process is handled online from your office.
Clarity: Receive clear, concise reports that are clinically relevant to chiropractic care, not generic medical reports.
Posted onTrustindex verifies that the original source of the review is Google. Kinetic radiology has been an absolute game changer in speed of reports and detailed reports. Any other doctors I send my reports to are amazed at the detail and the pathology that gets picked up. This is my one and only radiologist group, im thrilled.Posted onTrustindex verifies that the original source of the review is Google. Rishi provides an outstanding service—fast, reliable, and incredibly reassuring. He’s quick to respond, efficient in his work, and always takes the time to address any concerns with clarity and professionalism. I highly recommend his services to anyone looking for a dependable DACBR.Posted onTrustindex verifies that the original source of the review is Google. Prompt efficient service that is thorough and clear. Spinal information is top notch and I've had patients discover kidney stones and possible issues with a hip joint replacement loosening as incidental findings that supported both me and the patient above expectations.Posted onTrustindex verifies that the original source of the review is Google. Quick, accurate, and easy to work with. My new radiology team!Posted onTrustindex verifies that the original source of the review is Google. Excellent, timely reads. Invaluable for CBCTPosted onTrustindex verifies that the original source of the review is Google. Best turnaround time and thorough reports out of any radiologist I’ve seen or worked with!Posted onTrustindex verifies that the original source of the review is Google. Very detailed reports and quick service. Highly recommendedPosted onTrustindex verifies that the original source of the review is Google. Fast turn around time for the radiology reports! Thank you for making this process as seamless as possible!Posted onTrustindex verifies that the original source of the review is Google. I am a NUCCA chiropractor located in Wauankee Wisconsin and I can tell you Dr. Rishi is the only radiologist I’d work with. Sure there are many others in my area but when you want the best you go to the best. He is very easy to work with and always fast to respond and report. 100% recommend.Posted onTrustindex verifies that the original source of the review is Google. Kinetic Radiology is great! They were able to read and get a report written immediately. They are my go to company for any and all images that I need read!Load more
We service all 50 U.S. States, including the following States and Cities listed below.
Copyright 2024 Kinetic Radiology All Rights Reserved
Website Privacy | Terms of UseReceive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.
Copyright 2024 Kinetic Radiology
All Rights Reserved
Receive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.