A 42-year-old male who is presenting with several weeks of lower back pain. Initially, the pain was localized to his lower back and was somewhat intermittent, which he attributed to a weekend of yard work. However, over the past few days, the pain has intensified and now radiates down his left leg, specifically along the posterior aspect of his thigh and calf, sometimes even reaching his foot. This radiating pain is often described as sharp, shooting, or electrical, a classic sign of radiculopathy, indicating nerve root irritation.
He also reports associated symptoms such as numbness and tingling in his left foot, particularly in the lateral aspect and the third and fourth toes. He denies any significant weakness in his leg but mentions feeling a bit “clumsy” at times. His bowel and bladder function are normal. He has tried over-the-counter pain relievers with minimal relief. His past medical history is unremarkable, and he has no history of trauma.

The radiology report can be dense. Let’s translate it into what actually matters for our treatment plan. Think of the disc as a jelly donut.
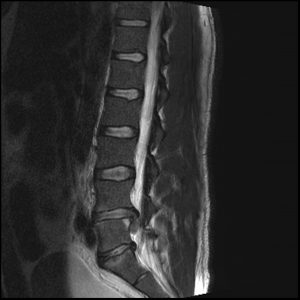
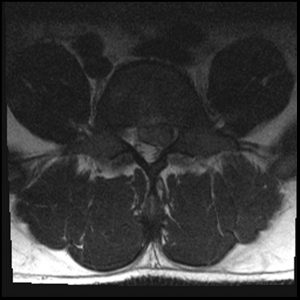
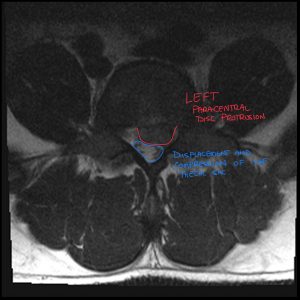
Our patient’s MRI confirmed a left paracentral disc extrusion at L4-L5, compressing the descending L5 nerve root. The MRI provided the anatomical confirmation of what our clinical exam already concluded. It adds value, but it doesn’t lead the dance.
To better grasp what’s happening, let’s briefly review the anatomy of the lumbar spine. The lumbar spine consists of five vertebrae (L1-L5) stacked upon each other. Between each vertebra lies an intervertebral disc, which acts as a shock absorber and allows for movement. Each disc has two main components:
Exiting from the spinal canal at each vertebral level are nerve roots, which branch off from the spinal cord and travel to different parts of the body. In Mr. Jones’s case, the pain radiating down his left leg suggests irritation or compression of one of the nerve roots in the lumbar spine, most likely in the L4-L5 or L5-S1 region, given the distribution of his symptoms.
The symptoms of a lumbar disc herniation can vary depending on the size and location of the herniation, as well as the specific nerve root being affected. Common symptoms include:
In Mr. Jones’s case, his left-sided radicular pain, numbness, and tingling in the lateral foot are classic symptoms of a possible lumbar disc herniation affecting the L5 or S1 nerve root.
While many cases of lumbar disc herniation can be managed conservatively, certain “red flag” symptoms warrant immediate attention and often necessitate referral to the emergency department or a neurologist. These red flags suggest potentially serious underlying conditions, such as cauda equina syndrome or progressive neurological deficits:
Magnetic Resonance Imaging (MRI) is the gold standard for imaging the soft tissues of the spine, including the intervertebral discs and nerve roots. It provides detailed images that can clearly visualize a disc herniation and its effect on the surrounding neural structures.
In this case, an MRI of the lumbar spine would likely be ordered. The radiologist interpreting the MRI will look for several key findings:
Radiologists use specific terminology to describe the type and extent of a disc herniation:
The MRI report will also describe the location of the herniation (e.g., central, paracentral, foraminal, extraforaminal) and its effect on the nerve roots. A paracentral herniation, for example, is located just to the side of the midline and is the most common type to cause radiculopathy. It will also specify which nerve root(s) appear to be compressed or displaced.
Conservative management is the mainstay of treatment for most symptomatic lumbar disc herniations, especially in the absence of red flags. This typically involves a multidisciplinary approach that may include:
Prompt referral to a neurologist or the emergency department is essential when red flag symptoms are present, as these may indicate a serious neurological compromise requiring urgent intervention.
Referral to the Emergency Department is warranted for:
Referral to a Neurologist is indicated for:
Empowering patients with knowledge about their condition is crucial for successful management. Patients with lumbar disc herniations should understand:
In a diverse healthcare setting, collaborating with a diagnostic imaging consultant, such as a DACBR chiropractic radiologist with expertise in musculoskeletal imaging, offers significant benefits:
Improved Communication and Clinical Correlation: Radiologists can provide crucial context, linking imaging findings to the patient’s clinical presentation
In a competitive healthcare environment, diagnostic precision is what sets a premier practice apart. Integrating Kinetic Radiology’s Diagnostic Imaging Consultants into your workflow is more than an alliance; it’s a strategic upgrade to your clinical authority and patient outcomes. Stop guessing and start knowing.
Unrivaled DACBR Expertise: Our reports are interpreted and written by board-certified chiropractic radiologists (DACBRs). As chiropractors who have completed years of specialized residency training in musculoskeletal diagnostic imaging, we understand your clinical perspective. We answer the questions you have because we speak your language, delivering insights a general radiologist might miss.
Accelerated Diagnostic Clarity: Eliminate the delays that create uncertainty. Our streamlined system delivers precise, actionable X-ray reports with industry-leading speed. This allows you to formulate confident treatment plans faster, improving patient throughput and satisfaction.
Enhance Your Standard of Care & Reputation: Position your practice as a leader in clinical excellence. Utilizing a DACBR service isn’t just outsourcing; it’s a direct investment in your standard of care. It demonstrates an unwavering commitment to diagnostic accuracy, which builds patient trust, strengthens your professional reputation, and mitigates clinical risk.
Don’t let diagnostic uncertainty limit your practice’s potential. Whether you’re facing a complex trauma case, require a definitive second opinion, or need reliable interpretation for routine X-rays, demand the highest standard.
Schedule your complimentary consultation with a Diagnostic Imaging Consultant today. Discover how our DACBR-level insights will immediately benefit your patients and solidify your clinical authority.
Rib fractures are hard to see on X-rays due to overlapping bones and soft tissues, subtle or non-displaced fractures, and the orientation of the fracture line, all of which can obscure the injury.
The main symptom is sharp, localized chest or rib pain that worsens with deep breathing, coughing, or movement. Patients may also experience tenderness, bruising, or a catching-like pain.
Yes, it’s very common to have a rib fracture that doesn’t appear on a standard X-ray. When this happens, advanced diagnostic imaging like a CT scan or ultrasound is crucial to confirm the injury and ensure proper management.
Modern teleradiology platforms make getting an expert second opinion simple, fast, and secure.
Find a Chiropractic Teleradiology Service: Choose a reputable service that is staffed by DACBRs. These platforms are designed specifically for chiropractors.
Securely Upload Patient Images: Export the DICOM files from your imaging software and upload them to the service’s secure, HIPAA-compliant online portal. You will also provide a brief clinical history for context.
Receive Your Detailed Report: The DACBR interprets the images and sends a comprehensive, actionable report directly to you, often within 24 hours. This report will clearly state the findings, impressions, and clinical recommendations.
Partnering with a DACBR teleradiology service provides more than just a second opinion; it offers a significant return on investment:
Speed: Get expert reports in hours, not days.
Expertise: Access board-certified specialists without having to hire them.
Convenience: The entire process is handled online from your office.
Clarity: Receive clear, concise reports that are clinically relevant to chiropractic care, not generic medical reports.
Posted onTrustindex verifies that the original source of the review is Google. Kinetic radiology has been an absolute game changer in speed of reports and detailed reports. Any other doctors I send my reports to are amazed at the detail and the pathology that gets picked up. This is my one and only radiologist group, im thrilled.Posted onTrustindex verifies that the original source of the review is Google. Rishi provides an outstanding service—fast, reliable, and incredibly reassuring. He’s quick to respond, efficient in his work, and always takes the time to address any concerns with clarity and professionalism. I highly recommend his services to anyone looking for a dependable DACBR.Posted onTrustindex verifies that the original source of the review is Google. Prompt efficient service that is thorough and clear. Spinal information is top notch and I've had patients discover kidney stones and possible issues with a hip joint replacement loosening as incidental findings that supported both me and the patient above expectations.Posted onTrustindex verifies that the original source of the review is Google. Quick, accurate, and easy to work with. My new radiology team!Posted onTrustindex verifies that the original source of the review is Google. Excellent, timely reads. Invaluable for CBCTPosted onTrustindex verifies that the original source of the review is Google. Best turnaround time and thorough reports out of any radiologist I’ve seen or worked with!Posted onTrustindex verifies that the original source of the review is Google. Very detailed reports and quick service. Highly recommendedPosted onTrustindex verifies that the original source of the review is Google. Fast turn around time for the radiology reports! Thank you for making this process as seamless as possible!Posted onTrustindex verifies that the original source of the review is Google. I am a NUCCA chiropractor located in Wauankee Wisconsin and I can tell you Dr. Rishi is the only radiologist I’d work with. Sure there are many others in my area but when you want the best you go to the best. He is very easy to work with and always fast to respond and report. 100% recommend.Posted onTrustindex verifies that the original source of the review is Google. Kinetic Radiology is great! They were able to read and get a report written immediately. They are my go to company for any and all images that I need read!Load more
We service all 50 U.S. States, including the following States and Cities listed below.
Copyright 2024 Kinetic Radiology All Rights Reserved
Website Privacy | Terms of UseReceive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.
Copyright 2024 Kinetic Radiology
All Rights Reserved
Receive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.