
As a chiropractor, you are on the front lines of musculoskeletal health. Patients present to your clinic every day with low back pain, but not all cases are simple mechanical issues. A young male patient walks in with persistent, deep, aching low back and buttock pain. It’s worse in the morning, lasting more than an hour, but strangely, it improves with exercise. Your clinical suspicion is piqued. Could this be more than a simple lumbar sprain? This classic presentation should raise a red flag for Ankylosing Spondylitis (AS), a condition where early and accurate diagnosis is critical for long-term patient outcomes.
Misinterpreting the subtle, early radiographic signs of AS can delay a crucial referral to a rheumatologist, potentially leading to irreversible joint fusion and disability. This is where the precision of an expert radiology interpretation becomes invaluable. For the modern chiropractic clinic, partnering with a specialized teleradiology service for chiropractors like Kinetic Radiology closes the diagnostic gap, providing you with the confidence to manage complex cases and ensure your patients receive the best possible care.
This guide will provide a deep dive into the imaging of Ankylosing Spondylitis, empowering you to identify key features and understand the vital role of expert chiropractic radiology in the patient’s journey.
Definition and Description Ankylosing Spondylitis is a chronic, progressive, inflammatory autoimmune disease belonging to a group of conditions known as the seronegative spondyloarthropathies. The term “seronegative” refers to the absence of rheumatoid factor in the blood, distinguishing it from rheumatoid arthritis. The hallmark of AS is inflammation of the axial skeleton, particularly the sacroiliac (SI) joints and the spine. This inflammation, known as enthesitis (inflammation where ligaments and tendons attach to bone), can lead to the gradual fusion of the vertebrae, resulting in a rigid, immobile spine.
Other Names for Ankylosing Spondylitis In medical literature and older texts, you may encounter other names for AS, which are useful to recognize:
Marie-Strümpell Disease
Bechterew’s Disease
Spondyloarthritis
The Clinical Picture: Who Gets AS and How Does It Manifest?
Clinical Context: Demographics Recognizing the typical patient profile is the first step in diagnosis.
Age: AS classically presents in young adults, with a peak onset between the ages of 20 and 30. Onset after age 45 is rare.
Sex: The condition has a strong male predilection, with a male-to-female ratio of approximately 3:1.
Genetics: There is a powerful genetic link. Over 90% of Caucasian patients with AS test positive for the human leukocyte antigen B27 (HLA−B27) gene. However, it’s important to note that many people with the HLA−B27 gene never develop AS.
Clinical Manifestations The patient’s history is revealing. Key symptoms include:
Insidious Onset: The pain begins gradually over weeks or months.
Inflammatory Back Pain: Characterized by morning stiffness lasting at least 30 minutes, improvement with gentle exercise or a hot shower, and worsening with inactivity or rest.
Sacroiliitis: Pain is often first felt deep in the gluteal region, corresponding to the sacroiliac joints.
Extra-articular Features: AS is a systemic disease. Be alert for signs outside the skeleton, including:
Acute Anterior Uveitis: Eye inflammation causing pain, redness, and blurred vision (occurs in ~40% of patients).
Inflammatory Bowel Disease (IBD): Crohn’s disease or ulcerative colitis.
Psoriasis: Skin and nail changes.
Cardiovascular Disease: Aortitis and aortic insufficiency can occur in late-stage disease.
Definitive Imaging Features of AS
Accurate Ankylosing Spondylitis imaging is the cornerstone of diagnosis. While labs like HLA−B27, ESR, and CRP are supportive, imaging reveals the structural changes that define the disease. An expert radiology interpretation can differentiate AS from its mimics and grade its severity.
X-Ray (Radiography) Findings & Buzzwords Radiography is the workhorse for initial evaluation. The disease process follows a predictable caudo-cranial path, starting at the SI joints and ascending the spine.
Sacroiliac Joints: This is where the story begins.
Early: Bilateral, symmetrical sacroiliitis is the hallmark. Look for indistinctness and blurring of the subchondral bone plate, primarily on the iliac side of the joint. This is known as pseudo-widening.
Intermediate: Sclerosis (increased density) appears around the joints, accompanied by erosions that create a jagged, “postage stamp” appearance.
Late: The erosions and sclerosis are replaced by complete bony fusion across the joint. The fused joint may be dense (ghost joint) or eventually disappear entirely.
Spine:
Romanus Lesions (“Shiny Corner Sign”): Early enthesitis at the insertion of the annulus fibrosus causes small erosions at the anterior corners of the vertebral bodies. The body’s healing response results in reactive sclerosis, creating a bright, “shiny” corner on radiographs.
Vertebral Squaring: The combination of corner erosion and periosteal new bone formation along the anterior vertebral body eliminates the normal anterior concavity, leading to a squared appearance.
Syndesmophytes: This is the key finding that differentiates AS from other spinal arthritides. In AS, inflammation of the annulus fibrosus leads to ossification, forming thin, delicate, vertically oriented bony bridges between vertebral bodies. These are marginal syndesmophytes as they arise from the edge of the vertebral body.
Bamboo Spine: In late-stage disease, the widespread formation of syndesmophytes across multiple levels, combined with apophyseal joint fusion, gives the spine its classic, undulating bamboo spine appearance.
Dagger Sign: Ossification of the supraspinous and interspinous ligaments on an AP view creates a single central radiodense line, known as the dagger sign.
Trolley-Track Sign: When the dagger sign is combined with ossification of the apophyseal joint capsules, it creates a three-line appearance (one central, two paramedian), known as the trolley-track sign.
Magnetic Resonance Imaging (MRI) Findings & Buzzwords Sacroiliitis MRI is the gold standard for early diagnosis, capable of detecting active inflammation years before changes are visible on x-ray. This is a critical point to communicate to patients and a primary reason to order advanced imaging.
Active Inflammatory Lesions (Best seen on STIR sequences):
Subchondral Bone Marrow Edema: The key finding of active sacroiliitis. This appears as a high signal (bright) on STIR sequences in the bone marrow adjacent to the SI joint.
Enthesitis & Capsulitis: Inflammation where ligaments and the joint capsule attach will also show high STIR signal.
Chronic/Structural Lesions (Best seen on T1 sequences):
Subchondral Sclerosis: Appears as low signal (dark) on all sequences.
Erosions: Bony defects along the joint margin.
Fatty Metaplasia: Fat deposition in the bone marrow post-inflammation appears as high signal (bright) on T1 images. This is a sign of previous inflammation.
Bony Ankylosis (Fusion): Visible as bridging bone marrow signal across the joint.
Computed Tomography (CT) and Ultrasound
CT: While not a primary diagnostic tool due to radiation dose, CT offers superior bony detail for assessing subtle erosions, fractures in a fused spine (see complications below), or pre-surgical planning.
Diagnostic Ultrasound: Its role in axial disease is limited. However, power Doppler ultrasound can be excellent for evaluating peripheral enthesitis, such as at the Achilles tendon or plantar fascia.
Complications: The Rigid Spine is a Fragile Spine
Spinal Fractures: The ankylosed spine is osteoporotic and brittle, behaving like a long bone. Even minor trauma can cause devastating fractures, often through the disc space (“carrot stick” fracture). An Anderson lesion is a pseudoarthrosis that develops at the site of a fracture or stress concentration.
Spinal Stenosis: Ossification of posterior ligaments can lead to narrowing of the spinal canal.
Osteoporosis: Chronic inflammation leads to significant bone density loss, increasing fracture risk.
Once AS is suspected based on your clinical evaluation and supported by expert radiology interpretation, a prompt referral is mandatory.
Referral: The patient should be referred to a Rheumatologist for definitive diagnosis, lab workup, and medical management.
Treatment: The rheumatologist will typically lead a multi-pronged approach:
Medications: NSAIDs are first-line. For progressive disease, Disease-Modifying Antirheumatic Drugs (DMARDs) and powerful biologics (e.g., TNF-alpha inhibitors) are used to control inflammation and halt progression.
Physical Therapy & Chiropractic Care: This is where co-management shines. Your role is vital for pain management, maintaining posture, and maximizing mobility in non-fused spinal segments. However, high-velocity, low-amplitude (HVLA) adjustments are strictly contraindicated over fused or acutely inflamed spinal segments due to the high risk of fracture. Precise imaging is non-negotiable for guiding safe treatment.
A rheumatologist will typically order baseline labs including HLA−B27, Erythrocyte Sedimentation Rate (ESR), and C−reactive protein (CRP).
Follow-up radiographs of the spine and pelvis are often taken every two years to monitor for structural progression.
In a case like Ankylosing Spondylitis, diagnostic ambiguity can have profound consequences. You need more than just a generic radiology report; you need a collaborative partner who understands the nuances of both chiropractic care and advanced musculoskeletal imaging. This is the core value of teleradiology for chiropractors.
Partnering with Kinetic Radiology provides:
Expertise on Demand: Direct access to a board-certified chiropractic radiologist who can identify the subtle signs of early sacroiliitis on an MRI or differentiate AS syndesmophytes from DISH osteophytes on an x-ray.
Increased Diagnostic Confidence: Eliminate uncertainty. Our detailed, actionable reports give you the confidence to make the right clinical decisions, whether it’s initiating appropriate conservative care or making a timely rheumatology referral.
Improved Patient Outcomes: Early diagnosis leads to early medical intervention, preventing irreversible fusion and disability. Your patients will thank you for your diagnostic diligence.
Reduced Liability: A definitive, expert interpretation of your imaging studies provides a powerful layer of medicolegal protection, especially when modifying treatment for high-risk conditions like AS.
Streamlined Workflow: Our easy-to-use platform provides fast, reliable teleradiology reporting, integrating seamlessly into your practice and allowing you to focus on what you do best: treating patients.
Conclusion: Elevate Your Practice with Expert Imaging Interpretation
Ankylosing Spondylitis is a complex systemic disease that often first presents in a chiropractic office. Recognizing the clinical pattern is the first step, but confirming the diagnosis and guiding safe treatment depends entirely on high-quality imaging and, most importantly, an expert interpretation. By understanding the key radiographic and MRI features—from the earliest signs of bone marrow edema to the late-stage bamboo spine—you position yourself as a true diagnostic authority.
Don’t let diagnostic uncertainty limit your practice’s potential or compromise patient care. Embrace the power of specialized teleradiology services.
A chiropractor is often the first healthcare provider to suspect AS based on the patient’s history and a thorough clinical exam. By ordering and correctly interpreting imaging (or partnering with a teleradiologist), they can arrive at a definitive working diagnosis. However, the formal diagnosis and medical management of AS should be done in co-management with a rheumatologist.
The most effective initial series includes an AP Pelvis view (to best evaluate both SI joints symmetrically) along with AP and Lateral views of the lumbar and thoracic spine. If these radiographs are negative or equivocal but your clinical suspicion remains high, the next and best step is an MRI of the sacroiliac joints without contrast, which can detect active inflammation (bone marrow edema) years before bony changes appear on x-ray.
It elevates your practice from a treatment-focused clinic to a true diagnostic hub. You benefit from faster, more accurate diagnoses, leading to better patient outcomes and increased patient trust. It reduces your professional liability by ensuring a specialist has reviewed complex imaging. Ultimately, it provides you with a trusted diagnostic partner, allowing you to practice with more confidence and authority.
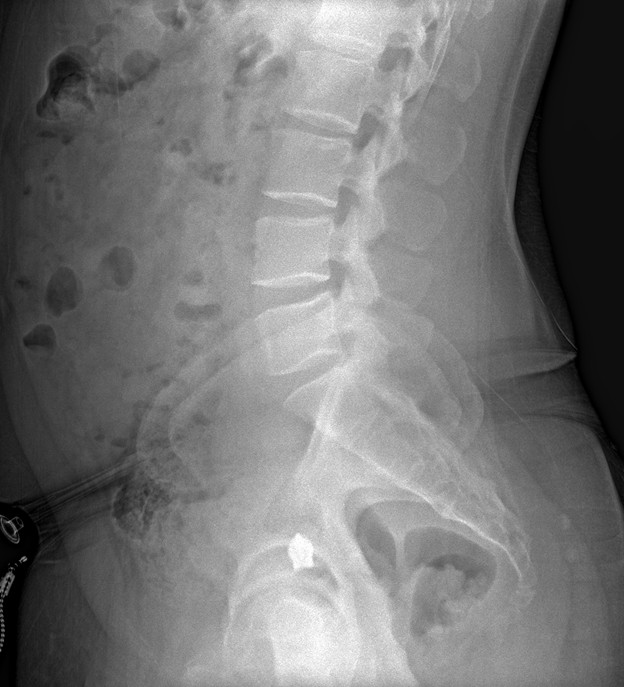
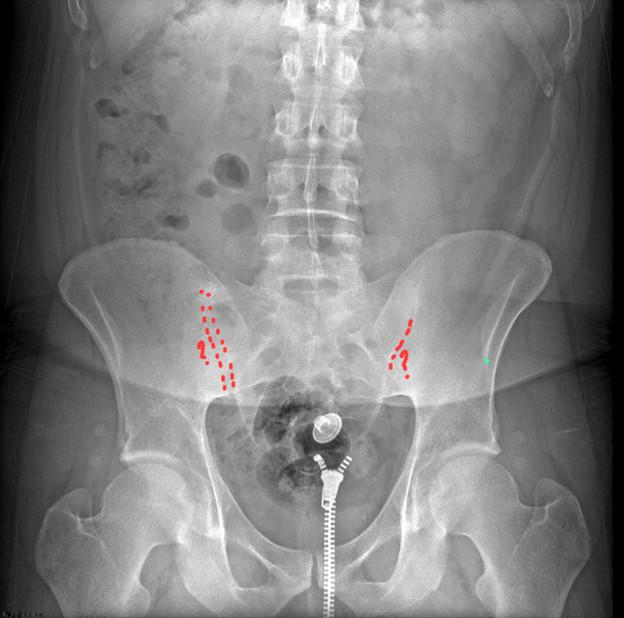
History: 30 Year Old Male with lower back pain.


The key radiographic finding on these images is the ankylosis seen involving the sacroiliac joints.
Posted onTrustindex verifies that the original source of the review is Google. Kinetic radiology has been an absolute game changer in speed of reports and detailed reports. Any other doctors I send my reports to are amazed at the detail and the pathology that gets picked up. This is my one and only radiologist group, im thrilled.Posted onTrustindex verifies that the original source of the review is Google. Rishi provides an outstanding service—fast, reliable, and incredibly reassuring. He’s quick to respond, efficient in his work, and always takes the time to address any concerns with clarity and professionalism. I highly recommend his services to anyone looking for a dependable DACBR.Posted onTrustindex verifies that the original source of the review is Google. Prompt efficient service that is thorough and clear. Spinal information is top notch and I've had patients discover kidney stones and possible issues with a hip joint replacement loosening as incidental findings that supported both me and the patient above expectations.Posted onTrustindex verifies that the original source of the review is Google. Quick, accurate, and easy to work with. My new radiology team!Posted onTrustindex verifies that the original source of the review is Google. Excellent, timely reads. Invaluable for CBCTPosted onTrustindex verifies that the original source of the review is Google. Best turnaround time and thorough reports out of any radiologist I’ve seen or worked with!Posted onTrustindex verifies that the original source of the review is Google. Very detailed reports and quick service. Highly recommendedPosted onTrustindex verifies that the original source of the review is Google. Fast turn around time for the radiology reports! Thank you for making this process as seamless as possible!Posted onTrustindex verifies that the original source of the review is Google. I am a NUCCA chiropractor located in Wauankee Wisconsin and I can tell you Dr. Rishi is the only radiologist I’d work with. Sure there are many others in my area but when you want the best you go to the best. He is very easy to work with and always fast to respond and report. 100% recommend.Posted onTrustindex verifies that the original source of the review is Google. Kinetic Radiology is great! They were able to read and get a report written immediately. They are my go to company for any and all images that I need read!Load more
We service all 50 U.S. States, including the following States and Cities listed below.
Copyright 2024 Kinetic Radiology All Rights Reserved
Website Privacy | Terms of UseReceive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.
Copyright 2024 Kinetic Radiology
All Rights Reserved
Receive timely resources to keep you and your practice on the cutting edge of Chiropractic Radiology.